Authors: Jennifer O’Brien and Marty Beneteau
When the buckets come out at Windsor Regional Hospital, chances are it’s raining outside.
Leaky roofs at both the Met and Ouellette campuses mean it’s not unheard of to have operating room surgeons navigate around pails on the floor during a heavy shower. They also have to worry about rainwater getting behind a wall, causing mould and compromising patient safety. Facilities staff work on high alert to prevent worst-case scenarios, such as a wet drywall ceiling giving way in the operating room.
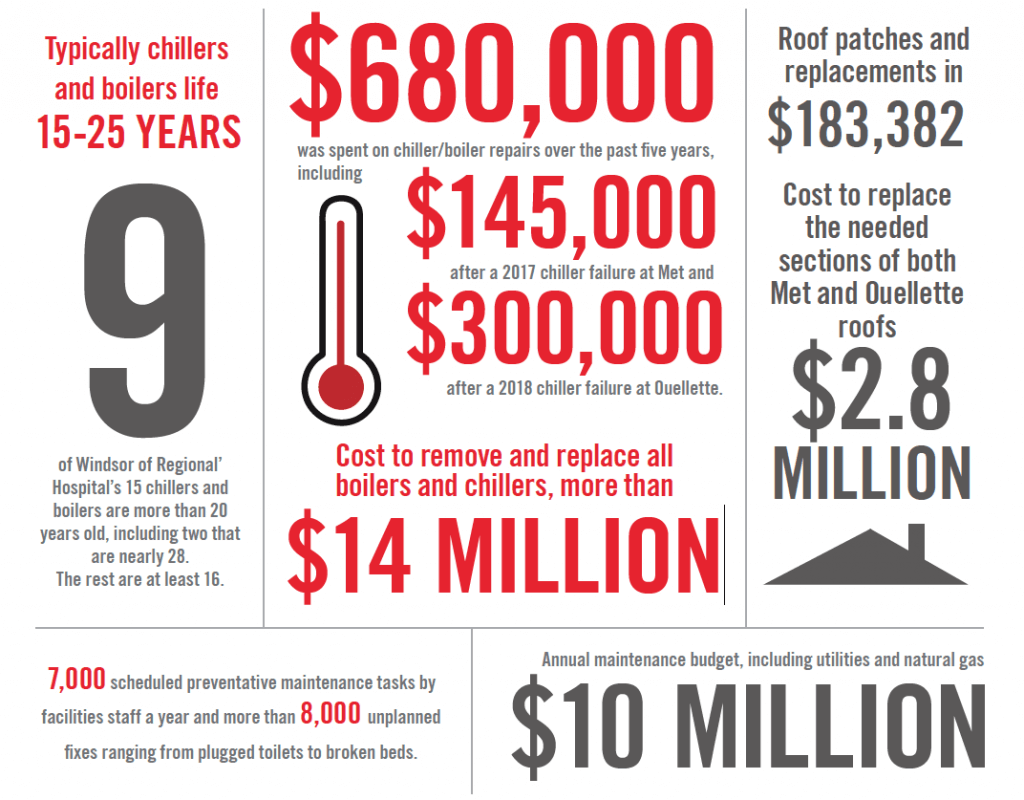
It would cost $2.8 million to replace both roofs, but because Windsor Regional is planning to move into a new building, the 20-year investment makes no sense. Instead, staff prowl the rooftops in search of breaches, patching as they go. In 2018, $183,000 that could have been spent on patient care went to roof leaks, says the hospital’s capital planning boss.
Seven years after agreeing to forego substantial capital investments in exchange for a one-time replacement hospital, such is the patchwork state of acute care in Windsor. It’s in critical condition.
“The issue is we have this really old infrastructure that we have to invest in just to keep the place going,” says Kevin Marshall, Windsor Regional’s director of corporate services and capital planning. “That’s money we aren’t spending on direct patient care.”
Leaky roofs aren’t the only big-ticket item. The hospital’s 15 boilers and chillers – million-dollar machines crucial to not only atmospheric comfort but sterilization and infection control – are nearing or past their best-before dates.
A boiler failure impacts “medical device reprocessing,” which means instruments can’t be cleaned and surgeries can get cancelled. Chillers bring cooling fluid to the air conditioning unit, which maintains temperature and humidity control and is critical for operating teams performing surgeries and for infection control.
In 2016 Windsor Regional cancelled and postponed about 300 surgeries due to failures in its sterilization systems at both campuses. The biggest issue occurred at Ouellette campus after aging-related problems in the 54-year-old piping that brings steam from the hospital’s powerhouse to the autoclaves which sterilize the instruments. “That was due to the age of the piping system,” says facilities manager John Faber.
“It’s not just about comfort. These are very critical pieces of equipment.”
It is estimated it would take $90 million to $100 million to address urgent issues ranging from roofs to drafty windows and boilers. This year, following a needs assessment by the province, Windsor Regional received $1.1 million under the Facility Condition Assessment Program.
Staff prepared a priority list and selected 20 of the “biggest headaches and (said) this is what we can afford,” within the allotted four-month period to spend the money, says Faber. The upgrades focused on patient safety. The list ranged from elevators at Ouellette ($72,000) to the nurse call system at Met ($144,000).
No bells and whistles
In 2015, an inspection found the fire alarm at Ouellette needed a substantial upgrade. Windsor Regional started a three-year project to replace the system at a cost of $2.1 million, but because of insufficient ceiling space the hospital could not include equipment needed for cutting edge features found in most modern hospitals.
“We couldn’t even go to the newest system,” says Faber. “No bells and whistles, no new features. You still just pull this lever and it still makes the bell ring. For $2.1 million.”
Some of the deficiencies may seem borderline comical. At Ouellette, where most of the patient rooms date back to 1962, there are hallways where an average-height adult can reach up and touch the ceiling. They have been dropped over the years to fit modern infrastructure, including ductwork and wiring needed to incorporate new technologies.
In some Windsor Regional wards, there aren’t enough outlets to plug in computers needed to meet today’s paperless standards.
‘A patchwork’
The buildings themselves are what Dr. Wassim Saad, chief of staff, calls a “patchwork” which date back decades. “Some of our hospital is between 80 and 100 years old,” says Saad. “Expansion is something we cannot do at either site because they are landlocked.”
Met was built in 1928. The first hospital at the Ouellette campus was built in 1888. Most of the patient rooms there were built between 1952 and 1962.
The hospitals have been maintained, repaired, expanded and renovated over the past century, including a major expansion at Met in 2004 and another at Ouellette in 2001 (expanding emergency services, operating rooms and the diagnostic imaging department).
But many features are still outdated – including windows and floors.
The clinical teaching unit at Ouellette was originally a pediatric unit. The rooms were meant for one child each. Now those same rooms house three adult patients at a time. “If I’m sitting in the middle of that room, I can almost touch all three beds at the same time,” says Saad.
The problem is most glaring when a patient is in crisis and an emergency or “code” team must rush into the room with a large cart full of supplies. It’s too crowded. Hospital staff need to get other patients – who are also very sick – into a hallway during the urgent situation, he says.
Hospital-acquired infections
Patient beds in semi-private rooms at Ouellette campus are 90 centimetres apart, about the width of a microwave oven, which is a concern to Windsor Regional’s manager of infection prevention and control.
“It’s close quarters,” says Erika Vitale. “When you start adding an IV pole, a chair, a visitor’s chair, it’s very difficult. We have had outbreaks of influenza and Norwalk virus. Those can spread easily because of close quarters.”
Between April and September, more than 200 Windsor Regional patients contracted antibiotic-resistant bugs. While most people carried the bug without becoming sick, 19 ended up with what are called “hospital-acquired infections,” says Vitale.

In at least 20 percent of the cases the only known risk factor was that the patient shared a room with someone else who had the bug. It’s a difficult statistic to control in a facility where 80 percent of ward rooms are shared by at least two patients. The Ontario standard for new hospitals is 20 percent.
While hospital officials won’t guess how the new building for the Windsor-Essex Hospitals System will change things, they expect the numbers to go down. The plan is for 80 percent of the rooms to be private and all of the bed spaces to have dedicated bathrooms, so the risk of exposure will decrease significantly, says Vitale.

The same goes for preventable outbreaks that have forced Windsor Regional to cancel surgeries in the past, says Vitale.
In 2018, Windsor Regional had to postpone 29 surgeries due to four outbreaks of the flu – two at the Ouellette campus and two at the Met campus.
Outbreaks occur when patients who are already in the hospital become infected by exposure to other patients. In 2018, four patients and six staff members were infected at Met campus, and nine patients and seven staff members at Ouellette, Vitale says.
The logistics at the old hospitals increase the risk of patients acquiring infections, because most patients share bathrooms, she says.
“When you have an enteric illness – vomiting, diarrhea – it’s very contagious. If you are sharing a bathroom with somebody, that’s how people pick it up. In the new hospital every patient would have their own toilet facility.”
When it breaks
- The inability to control extreme heat and humidity can play havoc. This past summer, $75,000 worth of disposable equipment was lost due to humidity in the Ouellette campus cystoscopy room.
- Anesthetic machines at the Ouellette campus operating room were ruined in 2014 by an outside water backup caused by an old, inundated system with a malfunctioning sensor and no redundancy. The replacement cost was $1.2 million.
- Operating room delays have been caused when equipment must be transferred between campuses and re-sterilized.
“What these numbers show is that these hospitals need investment just to maintain the status quo. But even if we had a blank check to invest in everything on the list, we are still operating in old, tired buildings, in two landlocked facilities, where patient privacy and infection control is a constant challenge. We need to move forward so our patients can have access to modern health care. The longer this project is delayed, the more money we will have to spend on projects that do nothing to improve the quality of care we are able to offer our patients.”
Windsor Regional Hospital CEO David Musyj
